Podcast: Play in new window | Download (Duration: 47:14 — 86.8MB)
Vitamin D is more important that we thought.
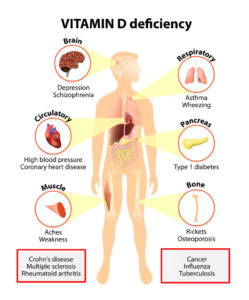
The medical literature currently contains more than 50,000 articles on Vitamin D. Vitamin D levels play a significant role in a number of systems in the body, including immune and neurological regulation, and bone health. When levels of this nutrient are low, that increases the risk of cancer and heart disease, autoimmune disorders and psychiatric and mood problems.
In addition, according to the National Institutes of Health, Vitamin D may play a role in prevention and treatment of Type 1 and Type 2 Diabetes, hypertension, glucose intolerance, multiple sclerosis, and other medical conditions.
Vitamin D:
- Moderates cell division — Vitamin D is a hormone whose function is to provide vital communication links between cells, to normalize cell growth and prevent aggressive cell production.
- Prevents autoimmune disorders —Control mechanisms are built into the immune system that prevent immune activity from causing damage due to inflammation— Vitamin D is essential to the function of these control mechanisms.
- Reduces inflammation in the brain and nervous system —Vitamin D moderates inflammatory processes in the neurological system. This is particularly important, since the brain lacks the regulatory systems to moderate inflammation effectively.
- Vitamin D levels are considered healthy when 50-80 ng/mL.
Most treatments involve more than a single approach. However, when Vitamin D is lacking, no other intervention will be 100% effective. Knowing Vitamin D status is essential to correct any depletion. Above content provide by PERQUE Integrative Health.
 Following excerpt from National Institutes of Health (NIH). “Vitamin D is a fat-soluble vitamin that is naturally present in very few foods, added to others, and available as a dietary supplement. It is also produced endogenously when ultraviolet rays from sunlight strike the skin and trigger vitamin D synthesis. Vitamin D obtained from sun exposure, food, and supplements is biologically inert and must undergo two hydroxylations in the body for activation.
Following excerpt from National Institutes of Health (NIH). “Vitamin D is a fat-soluble vitamin that is naturally present in very few foods, added to others, and available as a dietary supplement. It is also produced endogenously when ultraviolet rays from sunlight strike the skin and trigger vitamin D synthesis. Vitamin D obtained from sun exposure, food, and supplements is biologically inert and must undergo two hydroxylations in the body for activation.
Vitamin D promotes calcium absorption in the gut and maintains adequate serum calcium and phosphate concentrations to enable normal mineralization of bone and to prevent hypocalcemic tetany. It is also needed for bone growth and bone remodeling by osteoblasts and osteoclasts. Without sufficient vitamin D, bones can become thin, brittle, or misshapen. Vitamin D sufficiency prevents rickets in children and osteomalacia in adults. Together with calcium, vitamin D also helps protect older adults from osteoporosis.
Vitamin D has other roles in the body, including modulation of cell growth, neuromuscular and immune function, and reduction of inflammation. Many genes encoding proteins that regulate cell proliferation, differentiation, and apoptosis are modulated in part by vitamin D. Many cells have vitamin D receptors.
There is considerable discussion of the serum concentrations of 25(OH)D associated with deficiency (e.g., rickets), adequacy for bone health, and optimal overall health, and cut points have not been developed by a scientific consensus process.
Sources of Vitamin D
- Food. Very few foods in nature contain vitamin D. The flesh of fatty fish (such as salmon, tuna, and mackerel) and fish liver oils are among the best sources. Small amounts of vitamin D are found in beef liver, cheese, and egg yolks. Vitamin D in these foods is primarily in the form of vitamin D3. Some mushrooms provide vitamin D2 in variable amounts. Mushrooms with enhanced levels of vitamin D2 from being exposed to ultraviolet light under controlled conditions are also available.
- Sun exposure. Most people meet at least some of their vitamin D needs through exposure to sunlight. Complete cloud cover reduces UV energy by 50%; shade (including that produced by severe pollution) reduces it by 60%.
- Dietary supplements. In supplements and fortified foods, vitamin D is available in two forms, D2 (ergocalciferol) and D3 (cholecalciferol) that differ chemically only in their side-chain structure.
- Vitamin D Deficiency. Nutrient deficiencies are usually the result of dietary inadequacy, impaired absorption and use, increased requirement, or increased excretion. A vitamin D deficiency can occur when usual intake is lower than recommended levels over time, exposure to sunlight is limited, the kidneys cannot convert 25(OH)D to its active form, or absorption of vitamin D from the digestive tract is inadequate. Vitamin D-deficient diets are associated with milk allergy, lactose intolerance, ovo-vegetarianism, and veganism.
Groups at Risk of Vitamin D Inadequacy
Nutrient deficiencies are usually the result of dietary inadequacy, impaired absorption and use, increased requirement, or increased excretion. A vitamin D deficiency can occur when usual intake is lower than recommended levels over time, exposure to sunlight is limited, the kidneys cannot convert 25(OH)D to its active form, or absorption of vitamin D from the digestive tract is inadequate. Vitamin D-deficient diets are associated with milk allergy, lactose intolerance, ovo-vegetarianism, and veganism.
 Breastfed infants. Vitamin D requirements cannot ordinarily be met by human milk alone.
Breastfed infants. Vitamin D requirements cannot ordinarily be met by human milk alone.- Older adults. Older adults are at increased risk of developing vitamin D insufficiency in part because, as they age, skin cannot synthesize vitamin D as efficiently, they are likely to spend more time indoors, and they may have inadequate intakes of the vitamin.
- People with limited sun exposure. Housebound individuals, women who wear long robes and head coverings for religious reasons, and people with occupations that limit sun exposure are unlikely to obtain adequate vitamin D from sunlight.
- People with dark skin. Greater amounts of the pigment melanin in the epidermal layer result in darker skin and reduce the skin’s ability to produce vitamin D from sunlight.
- People with dark skin. Greater amounts of the pigment melanin in the epidermal layer result in darker skin and reduce the skin’s ability to produce vitamin D from sunlight.
- People with inflammatory bowel disease and other conditions causing fat malabsorption. Because vitamin D is a fat-soluble vitamin, its absorption depends on the gut’s ability to absorb dietary fat. Individuals who have a reduced ability to absorb dietary fat might require vitamin D supplementation.
- People who are obese or who have undergone gastric bypass surgery. A body mass index ≥30 is associated with lower serum Vitamin D levels compared with non-obese individuals; people who are obese may need larger than usual intakes of vitamin D to achieve levels comparable to those of normal weight.
- Osteoporosis. More than 40 million adults in the United States have or are at risk of developing osteoporosis, a disease characterized by low bone mass and structural deterioration of bone tissue that increases bone fragility and significantly increases the risk of bone fractures.
- Cancer. Laboratory and animal evidence as well as epidemiological data suggest that vitamin D status could affect cancer risk.
- Other conditions. A growing body of research suggests that vitamin D might play some role in the prevention and treatment of type 1 and type 2 diabetes, hypertension, glucose intolerance, multiple sclerosis, and other medical conditions. Excerpt from NIH article entitled Vitamin D – Fact Sheet for Health Professionals.
PERQUE D3 Cell Guard
 PERQUE D3 Cell Guard provides this safe and natural form of Vitamin D3 in a liquid form with Medium Chain Triglycerides (MCT) for effective uptake and absorption. Additional protection to the D3 is provided by mixed natural tocopherols and ascorbyl palmitate in a natural rosemary extract. Like every other PERQUE product, D3 Cell Guard comes with a 100%, unconditional, money-back guarantee – the strongest guarantee in the natural health industry.
PERQUE D3 Cell Guard provides this safe and natural form of Vitamin D3 in a liquid form with Medium Chain Triglycerides (MCT) for effective uptake and absorption. Additional protection to the D3 is provided by mixed natural tocopherols and ascorbyl palmitate in a natural rosemary extract. Like every other PERQUE product, D3 Cell Guard comes with a 100%, unconditional, money-back guarantee – the strongest guarantee in the natural health industry.
Every PERQUE product is activated with the same transporters that are used by nature and in food to ensure full bioavailability. The biologically preferred form of an ingredient is always used for enhanced activity. • Free of citrus, MSG, wheat/gluten, corn/zein/starch, dairy/casein/whey/ milk derivatives, yeast, soy, sulfate, phosphates (other than coenzymes), and preservatives. • No genetically modified organisms (GMOs). Unique post-production assays and clinical bioassays assure product integrity.
YOUR QUALITY ASSURANCE: Every PERQUE product is produced following or exceeding the FDA’s pharmaceutical GMP (Good Manufacturing Practices) regulations.
About Dr. Jaffe
Dr. Russell M. Jaffe received his BS, MD and Ph.D from the Boston University School of Medicine in 1972. He completed residency training in clinical chemistry at the National Institutes of Health (1973 – 1976), remaining on the permanent senior staff until 1979. He is board certified in Clinical Pathology and in Chemical Pathology. On leaving NIH Dr. Jaffe began a journey that sought to support the emerging field of Integrative and Regenerative Medicine.
Dr. Jaffe is CEO and Chairman of PERQUE Integrative Health (PIH). His dedication to the application of primary prevention and his commitment to providing superior nutraceuticals and autoimmune testing with clinical evidence of superior efficacy has made him a sought after speaker and leader in his chosen field.










{ 0 comments… add one now }